How to Provide Better Patient Care Via Powerful Listening
“Doctors are men who prescribe medicines of which they know little, to cure diseases of which they know less, in men of whom they know nothing.”—credited to Voltaire
Twenty-first century sleep medicine professionals live and work in an era of unprecedented pressure. Productivity demands are up, reimbursements are down, and patient-centered outcomes matter more than ever. As a result, clinicians must not only work faster than before, they must work better.
In this article, you’ll learn how to conduct an initial patient interview for maximum efficiency and effectiveness. Because insomnia patients are often the most challenging and time-consuming sleep patients, insomnia patients will be used as an example. But the powerful communication skills shared here will serve you well with all patients. By implementing these strategies right away, you will reduce frustration and enhance patient outcomes in all of your patient interactions. We’ll focus on the initial interview because it’s the most complex visit.
How to Begin a Sleep Assessment Efficiently, Every Time
Patient satisfaction and treatment adherence begin long before the clinician enters the exam room. Every interaction with your practice has the potential to impact patient perception and thus shape patient behavior. (For a discussion of how these distal factors impact PAP adherence, read my article “How to Maximize Your Patients’ Motivation for PAP,” available here: http://emersonwickwire.com/innovation/how-to-maximize-your-patients-motivation-for-pap). And when the patient finally meets you, everything about your presence matters.
Your attire, posture, diction, tone of voice, and smile are powerful contributors to your stimulus value as a professional and an expert. It’s important to maximize your stimulus value because it is in your patients’ best interest. This makes it much easier for you to begin to have an impact immediately.
To make a difference quickly, you need to become an expert in establishing rapport. And the most important step you can take to build trust during the first encounter is to make the encounter all about your patient. Your focus should be what matters to him. In other words, you must discover the real reason he is in your office.
First, Define a Carrot
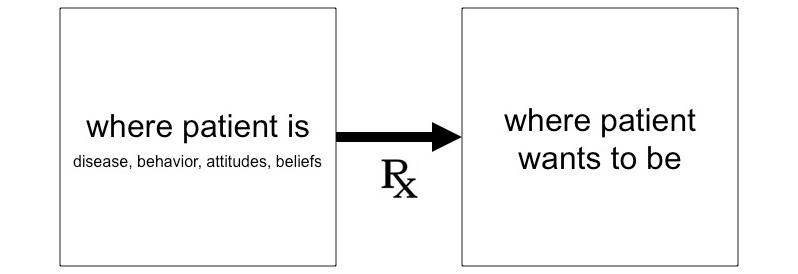
From a patient-centered perspective, the primary job of the sleep medicine clinician is to help patients move from where they are to where they want to be. This requires absolute clarity regarding the patient’s goals for treatment. What are the specific changes the patient seeks? How will these be manifested behaviorally? Identify these objectives first, then develop a treatment plan to achieve them.
In a recent companion article (http://emersonwickwire.com/innovation/how-to-talk-to-insomnia-patients-faster-more-effectively-and-with-less-frustration), I presented the Wickwire Funnel Framework (WFF) for improved expressive communication. The WFF provides three specific steps to help providers communicate faster, more effectively, and with less frustration; you must 1) frame the issue, 2) provide guiding principles, and 3) conclude with specific behavioral recommendations.
In similar fashion, structure is your friend when it comes to powerful and productive listening. In fact the most common provider mistake is asking a completely unstructured question such as, “What brings you to my office today?” From an efficiency and effectiveness perspective, starting with no clear direction is a devastating mistake! Instead, you need to quickly and effectively get to know what matters to your patient (hint: it’s not the apnea-hypopnea index!). As described in Table 1, there are three steps to the process. You must identify, clarify, and specify exactly what desired change will look like for your patients. Then you must include this specific change in your treatment plan and discharge instructions.
Here’s a simple sample dialog to show what defining a carrot looks like in action. The dozens of professionals whom I have trained in clinic report that since they have adopted this approach, they are routinely able to build trust, lower resistance, and get to know their patients within two minutes. Your patients will feel heard like never before, and your satisfaction ratings will improve.
You: As you know, I’m Dr Wickwire and a psychologist and sleep disorders specialist. We’re here to get your sleep on track. If I had a magic wand and could change anything about your sleep, what would that be?
Patient: I want to sleep through the night.
You: OK, if we achieved that, how would your life be different?
Patient: Hmmm…I’ve never thought about that. I wouldn’t wake up so tired, for one. And I’d have more energy during the day.
You: What would you do with that energy?
Patient: I’d exercise more.
You: What kind of exercise do you enjoy?
Patient: I used to love Pilates. There’s a class right near my house.
You: Great. So let me make sure I understand. If we help you sleep better through the night, you’ll have more energy during the day and will be able to get back to Pilates. Am I hearing that right?
Patient: Yes, that would be great.
You: Excellent. We can achieve that. Now let’s shift gears a bit and get started. In these next questions…
Table 1. Discovering the real reason patients are in your office.
| Objective | What to Say | What to Do |
| Identify | If I had a magic wand and could change anything about your sleep, what would that be? | Listen only |
| Clarify | If we were able to achieve that, how would you life be different? | Move toward concrete |
| Specify | If I were a fly on the wall and watching your life, what would that look like? | Specify concrete, measurable behaviors |
To maximize patient adherence and satisfaction, it’s not enough to ask about sleep-wake symptoms. You must help patients leverage sleep to improve the quality of their lives.
Keeping the Interview Moving
Once you’ve identified specific behavioral improvements in quality of life that healthy sleep can bring your patients, it’s time to shift into the history of present illness, medial history, and so on. But it’s always important to maintain focus and keep things moving toward the practical. From time to time, we’ve all had patients (or colleagues, bosses, or in-laws) who are hard to keep on track. One colleague refers to these patients as having a case of “rambling historiatitis.”
Without guidance, these well-intentioned patients will use forty words when three would suffice. For example, in response to your query regarding family history of sleep troubles, these patients are more likely to “think outloud” and present a complete genogram (including Aunt Myrtle’s astrological insights) rather than simply tell you that mom suffered insomnia and dad wears CPAP.
The problem in rambling historiatitis is that patients use too many words. Therefore, the solution is for patients to use fewer words. And like any disease, this is best achieved through prevention. If you want your patients to use fewer words, you must provide very specific instructions about how to answer you. Here are a few examples to get you started:
- In one sentence, tell me about your history of cancer.
- In three words or less [a range is OK], how long does it take for you to fall asleep at night?
- Yes or no, do you snore?
How to Close for Success, Satisfaction, and Sky-high Ratings
Other than opening the interview, winding down the encounter is the most important aspect of the interaction. Your patients will remember these final moments, which will have a disproportionate impact on future behavior. Cognitive psychologists refer to this as the “recency bias”—the human tendency to remember and ascribe more value to recent events relative to earlier events. As a result, it’s vital to adopt a clear and effective strategy to close the interview.
Your closing goals should be to verify your clinical impressions, solidify positive rapport, and to reiterate your specific behavioral recommendations for next steps. After you summarize your assessment, ask two questions:
- Does it feel like I’ve heard you correctly?
- Is there anything about your sleep that you think I should know, but haven’t asked?
These two questions are virtually guaranteed to ensure clinical accuracy and solidify your positive relationship. And from an efficiency perspective, here’s the kicker: if you follow the steps above, your patients will virtually never have anything additional to add!
Of course, your final discharge instructions must return to the carrot. To maximize adherence, you must provide a specific behavioral instruction to address the patient’s personal goals for treatment (eg, return to one Pilates class between now and next visit).
What to do Next
The practice of healthcare has never been more high-pressured. Extensive documentation of effectiveness is required. Clinical efficiency matters greatly. Yet sleep medicine remains an art as well as a science. Book learning and scientific understanding alone are insufficient. Instead, you need a proven system to communicate effectively and build rapport quickly. Employ the strategies and structure outlined above. You will help more patients faster than ever before, and you and your patients will be glad for it.